Which operation is performed on a thyroid gland depends upon 2 major factors: The first is the thyroid disease present that is necessitating the operation. The second is the anatomy of the thyroid gland itself as is illustrated below.
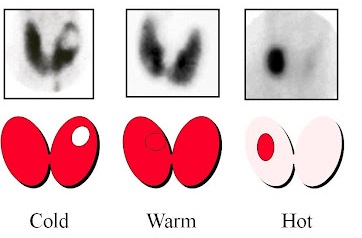
If a dominant solitary nodule is present in a single lobe, then removal of that lobe is the preferred operation (if an operation is even warranted). If a massive goiter is compressing the trachea and esophagus, the goal of surgery will be to remove the mass, and usually this means a sub-total or total thyroidectomy (occasionally a lobectomy will suffice). If a hot nodule is producing too much hormone resulting in hyperthyroidism then removal of the lobe that harbors the hot nodule is all that is needed.
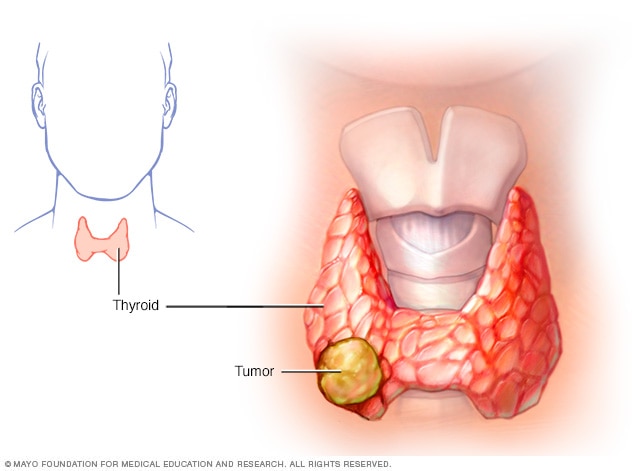
Most surgeons and endocrinologists recommend total or near total thyroidectomy in virtually all cases of thyroid carcinoma. In some patients with small papillary carcinomas, a less aggressive approach may be taken (lobectomy with removal of the isthmus). A lymph node dissection within the anterior and lateral neck is indicated in patients with well differentiated or follicular thyroid cancer if the lymph nodes can be palpated. This is a more extensive operation than is needed in the majority of thyroid cancer patients. All patients with medullary carcinoma of the thyroid require total thyroidectomy and aggressive lymph node dissection.
Surgical Options
Partial Thyroid Lobectomy
This operation is not performed very often because there are not many conditions which will allow this limited approach. Additionally, a benign lesion must be ideally located in the upper or lower portion of one lobe for this operation to be a choice.
Thyroid Lobectomy
This is typically the “smallest” operation performed on the thyroid gland. It is performed for solitary dominant nodules, which may be thyroid cancer or those which are indeterminate following fine needle biopsy . This surgery may also be appropriate for follicular adenomas, solitary hot or cold nodules, or goiters which are isolated to one lobe (not common).
Thyroid Lobectomy with Isthmusectomy
This simply means removal of a thyroid lobe and the isthmus (the part that connects the 2 lobes). This removes more thyroid tissue than a simple lobectomy, and is used when a larger margin of tissue is needed to assure that the “problem” has been removed. Appropriate for those indications listed under thyroid lobectomy as well as for Hurthle cell tumors, and some very small and non-aggressive thyroid cancers.
Subtotal Thyroidectomy
Just as the name implies, this operation removes all the “problem” side of the gland as well as the isthmus and the majority of the opposite lobe. This operation is typical for small, non-aggressive thyroid cancers. Also a common operation for goiters that are causing problems in the neck or even those which extend into the chest.
Total Thyroidectomy
This operation is designed to remove all of the thyroid gland. It is the operation of choice for all thyroid cancers which are not small and non-aggressive in young patients. Many surgeons prefer complete removal of thyroid tissue for all the different types of thyroid cancer.
Surgical Technique
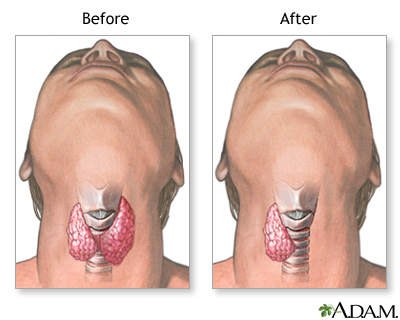
The standard neck incision is made typically measuring about 4 to 5 inches in length, although many endocrine surgeons are now performing this operation through an incision as small as 3 inches in thin patients. This incision is
made in the lower part of the central neck and usually heals very well. It is almost unheard of to have an infection or other problem with this wound. The surgeon will then typically remove part or all of the thyroid.
As mentioned above, for thyroid cancer, this will usually entail all of the thyroid lobe that harbors the malignancy, the isthmus, and a variable amount of the opposite lobe (ranging from 0% to 100%, depending on the size and aggressive nature of the cancer, the cancer type, and the experience of the surgeon). The surgeon must be careful of the recurrent laryngeal nerves, which are very close to the back side of the thyroid and are responsible for movement of the vocal cords. Damage to this nerve will cause hoarseness of the voice, which is usually temporary but can be permanent. This is an uncommon complication (about 1% to 2% of patients experience this), but it it is serious.
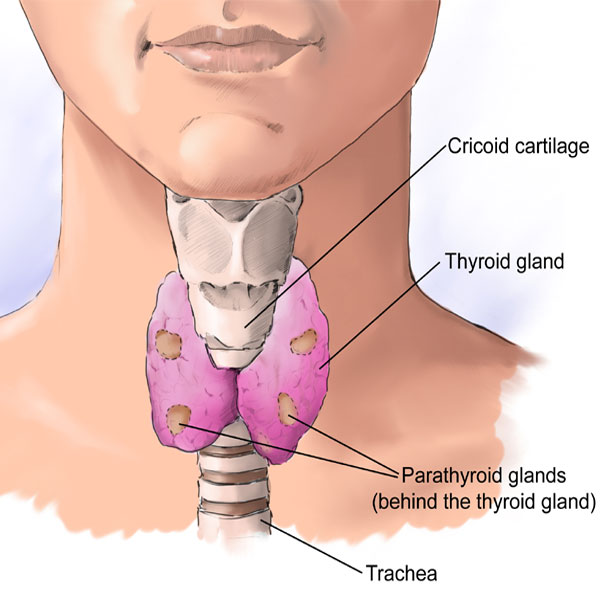
Your surgeon must also be careful to identify the parathyroid glands so their blood supply can be maintained. Another potential complication of thyroid surgery—although incredibly rare is—hypoparathyroidism, which is due to damage to all 4 parathyroid glands. Usually the only thyroid operations that have even a slight chance of this complication is the total or subtotal thyroidectomy. Although these complications can be serious, their risk should not be the sole determinant of whether or not to undergo surgery.
The relationship of the thyroid gland to the voice box and parathyroid glands in the image at right can be seen quite clearly. Remember that they share the same blood supply, so the surgeon must take care to preserve the parathyroid artery and vein while ligating the vessels to the thyroid gland itself. This is usually not a problem, but sometimes it is not possible to save them all. In this case, the surgeon will usually implant the parathyroid gland into a muscle in the neck. The parathyroid will grow there and function normally.
Often, formal thyroid surgery is not needed to determine if a thyroid mass is cancerous. Because these masses can often be felt, a physician can stick a small needle into it to sample cells for malignancy. This is called fine needle aspiration (FNA) biopsy. Don’t be afraid to ask questions if you don’t understand something.
